Insulin Resistance and Menopause: What You Need to Know
What Is Insulin Resistance?
Insulin resistance (IR) is a metabolic condition in which your cells don’t respond well to insulin. When cells become resistant, the body compensates by producing more insulin to keep blood sugar within a normal range. Over time, this high-insulin state disrupts metabolism, affects weight, and increases the risk of several chronic diseases.
Why Insulin Resistance Becomes More Common During Menopause
During perimenopause and menopause, estrogen levels naturally decline. Estrogen plays a key role in how the body uses insulin, stores fat and regulates inflammation. As estrogen drops:
The body becomes less responsive to insulin
Fat storage shifts toward the abdominal area
Blood sugar becomes harder to regulate
Weight gain happens more easily—even without significant lifestyle changes
You might notice symptoms such as increased belly fat, sugar cravings, energy crashes after meals, or feeling like weight loss requires twice as much effort.
How Insulin Resistance Is Diagnosed
Early IR often goes unnoticed because routine labs like fasting glucose and A1C may remain normal for years. To detect it earlier and more accurately, additional markers are helpful:
Key Tests and Indices
Fasting Insulin: Often elevated long before blood sugar rises
HOMA-IR: A calculation based on fasting glucose + fasting insulin; reflects the degree of insulin resistance
Triglyceride/HDL Ratio: Higher ratios are associated with metabolic dysfunction
TYG Index (Triglyceride–Glucose Index): Calculated using fasting triglycerides and fasting glucose; a sensitive marker for early IR and metabolic health
Fasting Glucose: Often normal initially, but included as part of the overall picture
Stages of Insulin Resistance
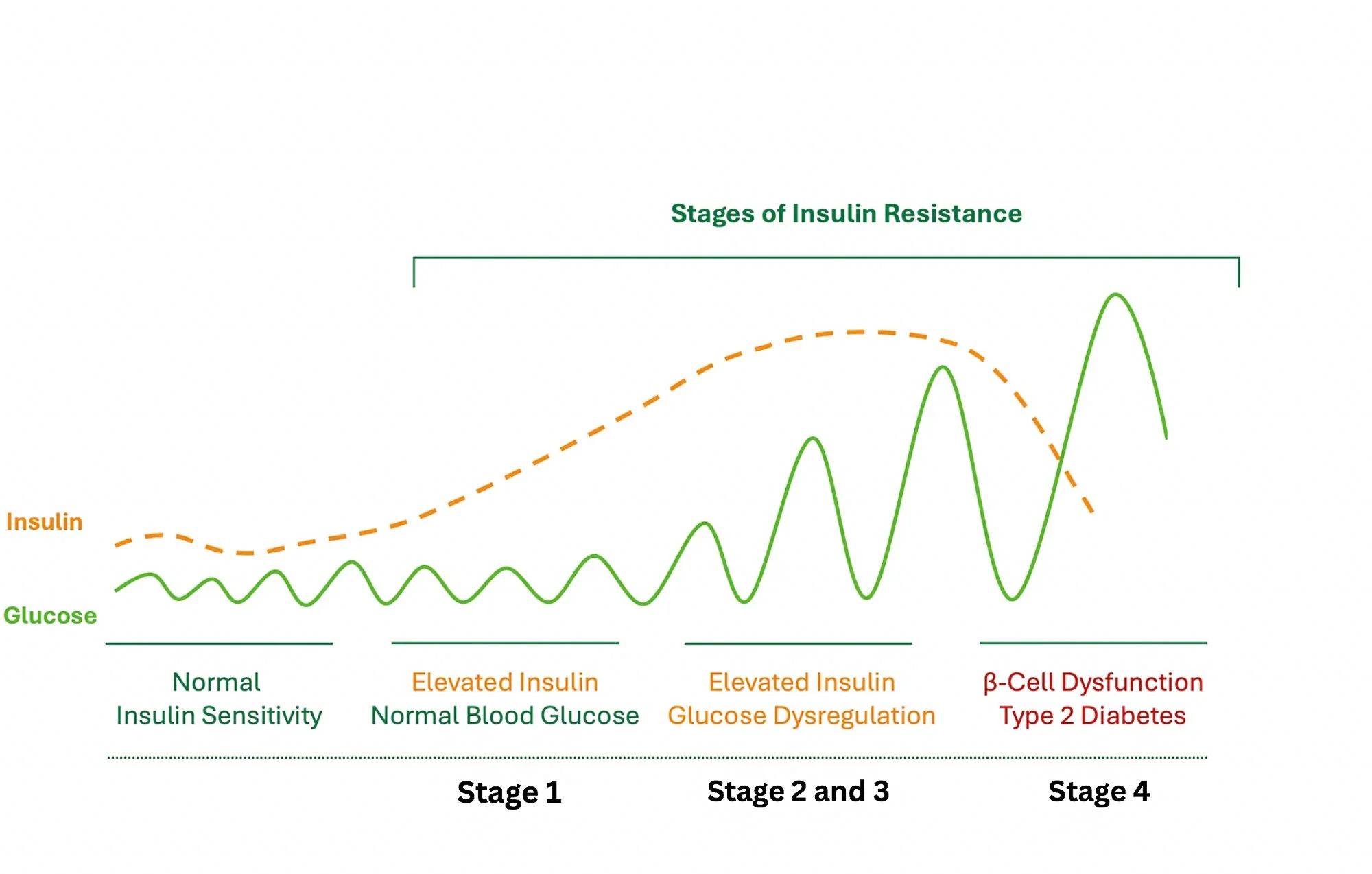
Insulin resistance doesn’t happen overnight. It progresses in stages, often silently, long before diabetes develops, as shown in the figure below.
1. Early (Compensated) Insulin Resistance
Cells respond less effectively to insulin
The pancreas produces extra insulin to maintain normal blood sugar
Labs: Normal glucose and A1C, elevated fasting insulin, elevated HOMA-IR
Symptoms: Belly fat gain, cravings, fatigue after meals
This is the most reversible stage.
2. Moderate Insulin Resistance (Hyperinsulinemia)
Insulin stays elevated throughout the day
Glucose may start trending upward
Labs: Worsening triglyceride/HDL ratio; high fasting insulin
Symptoms: Weight gain despite healthy habits, afternoon crashes, increased appetite
Chronic high insulin increases inflammation and cardiometabolic risk.
3. Dysglycemia (Prediabetes)
The pancreas struggles to keep up
Blood sugar begins to rise
Labs:
Fasting glucose 100–125 mg/dL
A1C 5.7–6.4%
Insulin still elevated
Still reversible with targeted lifestyle interventions.
4. Type 2 Diabetes
The pancreas becomes exhausted
Insulin production can no longer meet demand
Labs:
Fasting glucose ≥126 mg/dL
A1C ≥6.5%
Medication is often needed alongside lifestyle changes.
Why Early Diagnosis Matters
Lower disease risk: IR is linked to cardiovascular disease, fatty liver, dementia, and several cancers
Better outcomes: Early detection allows more effective and faster reversal
Improved quality of life: More stable energy, easier weight management, better hormonal balance during menopause
How to Improve Insulin Sensitivity
Evidence-based lifestyle strategies can significantly improve or reverse IR:
1. Healthy Eating
Focus on whole, unprocessed foods.
Reduce refined carbs and added sugars: Cut back on sweets, soda, white bread, and pastries.
Choose high-fiber carbs: beans, lentils, oats, quinoa, fruits, and vegetables.
Include lean protein that is low in saturated fat: fish, chicken, beans, tofu, unsweetened soy milk, edemame
Eat healthy fats in moderation: avocados, nuts, olive oil, fatty fish.
Impact: Can improve blood sugar control and reduce insulin levels within weeks.
2. Regular Physical Activity
Aerobic exercise (brisk walking, cycling, swimming): Aim for at least 150 minutes/week.
Strength training: 2–3 sessions per week helps build muscle, which improves how your body uses glucose.
Even short bouts of activity (like a 10-minute walk after meals) help lower blood sugar.
Impact: Exercise improves insulin sensitivity immediately and lasts for up to 48 hours after a workout.
3. Weight Management
Losing even 5–10% of body weight can significantly reduce insulin resistance.
Focus on sustainable habits, not crash diets.
Impact: Weight loss can improve insulin sensitivity and lower diabetes risk by more than 50% in people with prediabetes.
4. Better Sleep
Aim for 7–9 hours of quality sleep per night.
Poor sleep increases insulin resistance and hunger hormones.
Impact: Improving sleep can enhance insulin sensitivity in as little as 1–2 weeks.
These habits support healthy metabolism at any age, but they become especially important during menopause.